Accounts Receivable Report Types
By offering A/R services, pharmacies like KJ’s Pharmacy prioritize customer ease and accessibility, fostering strong relationships and providing essential support to their valued patients. Enables you to assess the financial state of the practice including the ability to drill all the way down to individual outstanding claims. It can also cause unnecessary write-offs, which means the provider will have to absorb that debt.
The Key to Efficient Accounts Receivable Management: Automation
Healthcare companies can guarantee that their AR procedures continue to be effective and financially viable by regularly adhering https://arslan.titanconnector.com/2022/06/17/audit-trails-critical-for-digital-evidence/ to these guidelines. It’s a gauge to see how much you’re losing in revenue because of untimely filing and uncollected debt. If your net collection rate is lower than 95 to 100 percent after write-offs, it means you’re doing poorly. Calls to Provider Relations are time-consuming and not consistently successful. Medicare Advantage plans have an escalation process like Medicare and can often be handled through online submission.

Top 5 Challenges in Home Health Billing & How to Overcome Them
That can be cumbersome and time-consuming if you’re still using manual processes and systems. Without tools that make it easy to capture this information, you risk claims rejections and denials down the line, which delay bill payment and affect liquidity. The balance remaining after the insurance provider has paid their share becomes the patient’s responsibility. Effective communication strategies, understanding patient financial situations, and offering flexible payment plans can greatly enhance the likelihood of collecting these balances. Invoice reminder software automates the process of sending payment reminders to patients. This can help ensure timely payments and reduce the administrative burden of manual follow-ups.

UME: Council on Medical Education reports & issue briefs
Coding errors, where incorrect medical codes are used in the claim, can lead to delays or denials of payment. Claim denials, where the insurer accounts receivable log for individual patients refuses to pay for the service rendered, can lead to an increase in AR and potential bad debt. These unique challenges necessitate specialized AR strategies in medical practices.
Consequently, high AR can lead to cash flow problems, impacting the practice’s ability to cover operational expenses, invest in new equipment or training, and ultimately provide the best possible patient care. For a long time if the account goes uncollected then the provider suffers not only loss of revenue but needed to set aside resources for collection. Moreover, staff should be aware of those Medicare patients who don’t possess co-insurance and these staff should collect the co-payment before the patient leaves the office. Our streamlined payment posting process enables you to process payment and adjustment transactions on multiple accounts within a batch, allowing for an efficient process when focusing on legacy accounts. This feature is conducive to an environment where billers can focus more of their valuable time on working down their current AR, while not sacrificing revenue from older accounts. Despite its significance, managing AR presents several difficulties for healthcare businesses.
The Ultimate Guide To Accounts Receivable Process
- Sending out payment reminders, post-due notices, formal dunning letters, and legal notices is a vital function of your AR team.
- If a claim is not paid by 90 days, there is a problem and the clock is ticking to get it resolved.
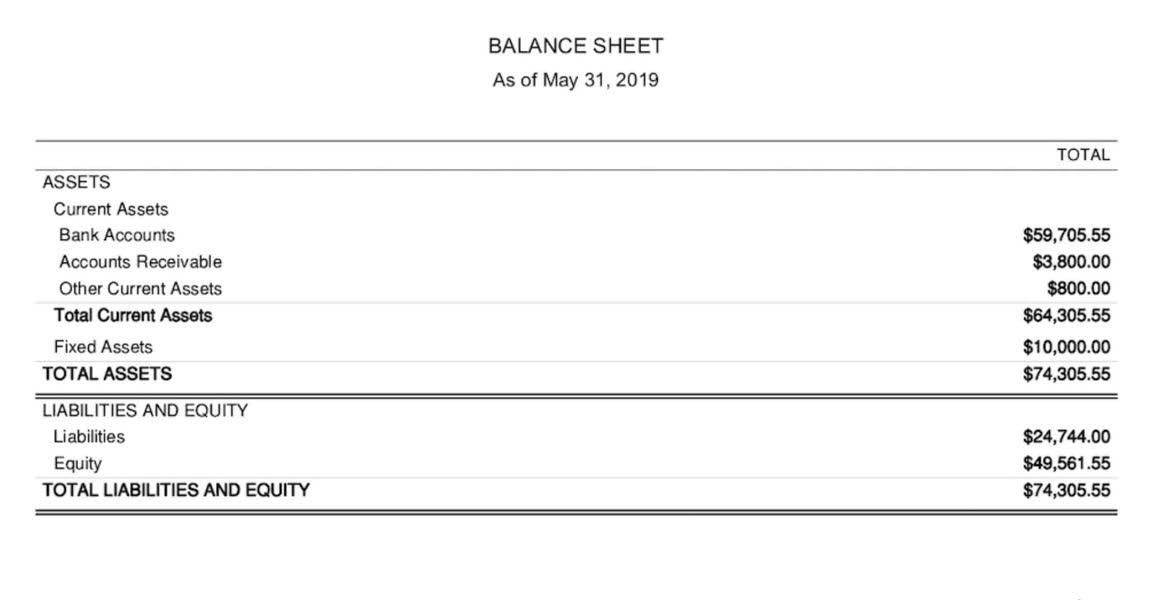
- The majority of A/R accounts at KJ’s Pharmacy are held by patients residing in nursing homes.
- It represents the amount of money that is due and should be collected within a specific timeframe, usually within a year.
- Dunning letters are communication tools that remind customers or clients about overdue payments.
- Coding errors, where incorrect medical codes are used in the claim, can lead to delays or denials of payment.
Physician practices can improve efficiency and reduce costs by implementing practice management system software that can automate a significant amount of revenue cycle functions. To help practices evaluate their needs and make informed choices when selecting a practice management system, the AMA and the Medical Group Management Association have created a collection of informational resources. Remember to review patient aging reports regularly and have set days to check the patient balances. If these steps are only partially successful, partnering with an agency for severe debt collections is always possible.

Tips from the industry to reducing AR days
AR plays a vital role in maintaining a healthy cash flow, which is integral to the overall financial health of a medical practice. The longer the duration between the provision of medical services and the receipt of payment, the higher the AR balance. Nowadays we observed that various factors that cause overheads for healthcare organizations such as outstanding claims and delayed collections as well as stringent federal regulations.
The Data Freshness date/time will let you know how current the information is. Don’t take “no” for an answer if supporting documentation is available for the claim. Furthermore, do not repeat an appeal step; go up to the next level of appeal and continue to escalate as needed. For those people who can’t afford to pay, update your financial hardship program. Use the Federal Poverty Level (FPL) Guidelines what are retained earnings as the standard for financial hardship.
- Accurate information from insurance to demographics starts at the front desk check-in process.
- A comprehensive accounts receivable log should provide clear and concise records of patient interactions, including payment dates, amounts due, and any communication with patients regarding their balances.
- In today’s fast-evolving healthcare landscape, the process of billing and collections has grown increasingly complex.
- An automated AR system allows accounts receivable officers to keep track of payments and track bills as they near their due date.
- Fortunately, there are some helpful steps for making the collections process a bit easier.
- The aim is to empower healthcare providers with the knowledge and tools needed to optimize their AR processes for better financial stability and success.
How can medical practices manage claim denials effectively?
Younger money is easier to get because supporting documentation is more readily available. Spending time on oldest accounts is not as fruitful because of the worry about expiration of timely filing. Displays the last payment made by the responsible party (insurance or patient).













